At-Home COVID-19 Tests: What You Need to Know About Your Plan, Rates, and More
By Carolyn Locke | Published January 13, 2022
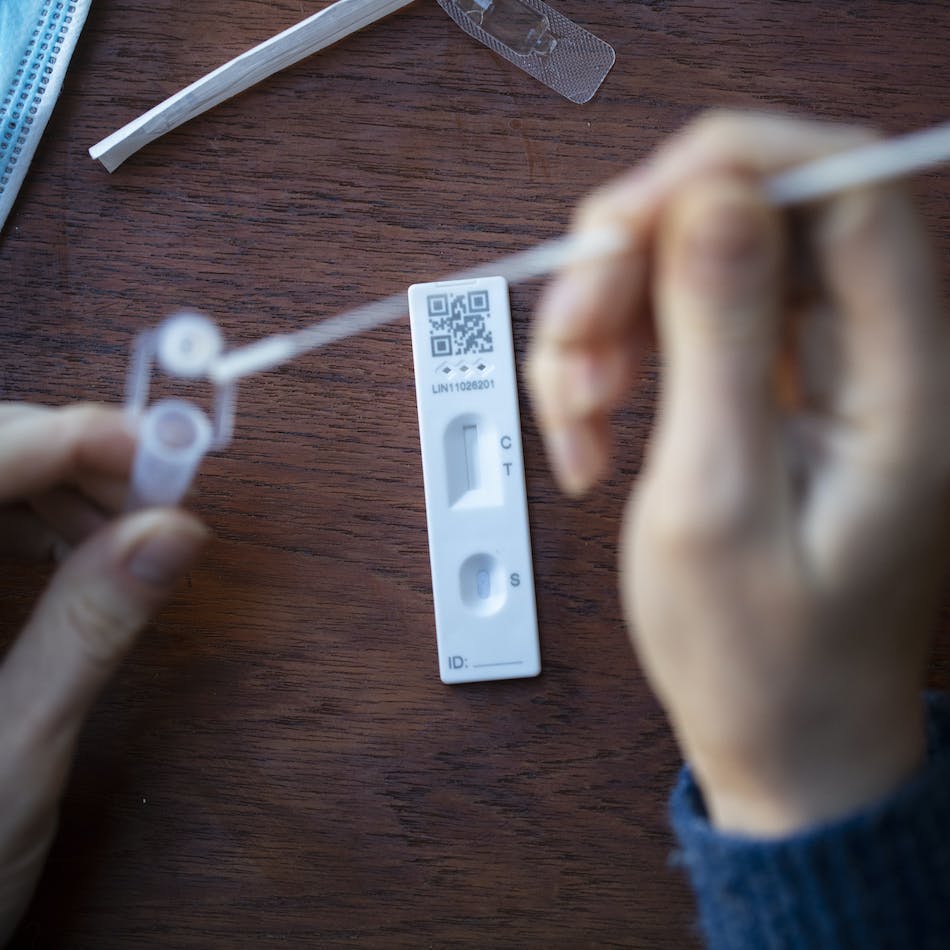
At-home COVID-19 tests are rapidly becoming a staple for Americans. Antigen tests are available at relatively low costs–usually ranging from 5-40–and these tests are generally more easily accessible and deliver rapid results compared to traditional PCR tests. These tests are incredibly convenient and a great option for those who want to ensure they are safely reporting to work or gathering with friends and family. Now, thanks to a recent announcement from the White House, starting this Saturday, January 15th, these at-home tests will be covered at no cost under medical plans for Americans with private health insurance.
While it is great news that these tests will be covered by insurance, currently the largest hurdle is availability. Due to the rise of Omicron cases, rapid tests have become more challenging to locate in stores. However, the President has committed to using the Defense Production Act (DPA) to ramp up the production of additional at-home rapid tests through two testing manufacturers.
Details are still emerging about the program, testing coverage, and administrative procedures. The Newfront team is here to help our clients understand how to best deploy an at-home testing program and any impact it may have on plans and rates.
Under the new mandate, at-home testing coverage for up to eight tests per person, per month will be provided under employer plans and for individuals who have purchased plans from the Affordable Care Act Exchange Marketplace. For example, a family of four that is covered under a private healthcare plan will have access to up to 32 tests, or eight per insured, at no cost to them. No prior authorization or doctor involvement is needed. The IRS has already stated that Covid testing coverage will never affect HDHP status or HSA eligibility.
Providers are encouraged to provide direct coverage for these over-the-counter tests. This will help mitigate the need for participants to pay up front and submit a claim with the receipt for reimbursement. However, under the guidelines, insurance companies are permitted to require plan participants to pay up front and submit a claim with the receipt for reimbursement.
The new guidelines only apply to at-home tests that are not employer-required. Insurance companies are not required to provide coverage where COVID-19 testing is for employment purposes, such as return-to-work or workplace screening testing. PCR and rapid tests taken on-site at a healthcare provider will continue to be covered and have no monthly limit.
Here is what is currently unclear: Past tests will likely not be eligible for reimbursement and it is unknown which tests will be covered moving forward.
The potential cost impact to healthcare plans is currently unknown The White House recently purchased 500 million rapid tests, but the insurance carriers have not officially confirmed whether the cost of tests will be covered by the government, or whether they will impact the medical loss ratio of the employer’s health plan. If the tests ultimately are determined to be billed back to the plan, this could potentially mean there are uncapped costs associated with this program. If that is the case, this could lead to an impact on future healthcare plan rates. While some plans, such as small, community-rated groups, may be less impacted than others due to not tracking specific employer claims data, cost impact will be determined by group size, company participation, and how an insurance company’s overall pool performs.
Until more information is made available, we cannot accurately project impact on plan rates and premiums.
At Newfront, we are actively monitoring the situation and will continue to post updates, including carrier-specific information, as information becomes available. COVID-19 Resources page.
In the meantime, check out our Compliance Alert that provides an FAQ on OTC Coverage mandate, and please don’t hesitate to reach out to your dedicated Newfront Employee Benefits team to learn more about bulk and competitive pricing for at-home COVID-19 testing solutions.

Carolyn Locke
Senior Vice President
Carolyn brings over 20 years of experience in benefits consultancy and human capital management systems technology to Newfront and her clients. Her knowledge in flexible benefits, long-term cost-containment strategies, commitment to a holistic approach when collaborating with clients on total reward programs makes her an essential partner to her clients. Carolyn’s unique background provides her clients with expertise in system integrations and implementations to improve the entire employee onboarding and offboarding process for a better employee experience.
Connect with Carolyn

